
Uncovering the Connection Between ADHD and Dopamine: A Neurological Perspective
ADHD, characterised by inattention and hyperactivity, is a complex neurological condition that affects millions worldwide. In recent years, researchers have delved into the intricate relationship between ADHD and dopamine, a key neurotransmitter in the brain’s reward system. This exploration has unveiled fascinating insights into how dopamine dysregulation may contribute to the symptoms of ADHD.
From impulsivity to poor concentration, the manifestations of ADHD could be tied to irregularities in dopamine pathways, altering behaviour and cognition. By understanding this connection, we gain a deeper appreciation of the neurological mechanisms underpinning ADHD and potential avenues for more targeted treatment approaches.
Join us as we navigate the intricate landscape of ADHD and dopamine from a neurological perspective, shedding light on how these two entities intersect and influence each other in the intricate dance of brain function.
Understanding ADHD and Dopamine
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterised by a range of symptoms, including inattention, hyperactivity, and impulsivity. Affecting both children and adults, ADHD can significantly impact daily functioning, academic performance, and interpersonal relationships. The complexities of ADHD extend beyond behavioural symptoms; they encompass a multitude of neurological factors that contribute to the disorder.
Dopamine, a critical neurotransmitter in the brain, plays a vital role in regulating mood, behaviour, and cognition. Its function is particularly important in the context of the brain’s reward system, influencing motivation and reinforcement of behaviours. Research has increasingly linked ADHD to anomalies in dopamine signalling pathways, suggesting that disruptions in dopamine levels may underlie some of the hallmark symptoms of the disorder.
Understanding the relationship between ADHD and dopamine involves exploring how dopamine influences attention, motivation, and executive function. When dopamine levels are insufficient or poorly regulated, individuals may experience challenges in sustaining attention, controlling impulses, and managing hyperactive behaviours. This intersection of ADHD and dopamine reveals a complex interplay that warrants further investigation to enhance our understanding of the disorder.
The Role of Dopamine in the Brain
Dopamine is often referred to as the “feel-good” neurotransmitter, but its role in the brain extends far beyond mere pleasure. It is involved in regulating various functions, including movement, cognition, mood, and emotional responses. Dopaminergic pathways, particularly those in the mesolimbic system, are crucial for the brain’s reward system, which reinforces behaviours that are essential for survival and well-being.
When dopamine is released in response to rewarding stimuli, it creates a sense of pleasure that motivates individuals to repeat the behaviour. This mechanism is essential for learning and habit formation. However, disruptions in dopamine signalling can lead to a range of issues, including addiction, mood disorders, and, notably, ADHD. In individuals with ADHD, the dysregulation of dopamine pathways can manifest as difficulties in reward processing, contributing to symptoms such as impulsivity and lack of sustained attention.
The balance of dopamine is critical for optimal brain function. An increase in dopamine in certain areas of the brain can enhance focus and motivation, while deficiencies in other regions may lead to cognitive impairments. In ADHD, the challenge lies in maintaining this delicate balance, as both excess and deficiency can lead to behavioural and cognitive disruptions. Understanding the multifaceted role of dopamine in the brain is fundamental to uncovering its connection to ADHD.
Neurological Implications of ADHD
The neurological implications of ADHD are extensive, involving multiple brain regions and circuits that govern attention, behaviour, and emotional regulation. Neuroimaging studies have shown that individuals with ADHD often exhibit structural and functional differences in areas such as the prefrontal cortex, basal ganglia, and cerebellum. These regions are closely associated with executive functions, impulse control, and motor activity, providing a neurological basis for the symptoms observed in ADHD.
Imbalances in neurotransmitters, particularly dopamine and norepinephrine, have been implicated in the pathophysiology of ADHD. The prefrontal cortex, responsible for decision-making, planning, and regulating social behaviour, relies heavily on dopaminergic activity. Insufficient dopamine levels in this region can lead to challenges in maintaining attention and inhibiting impulsive actions. Furthermore, the basal ganglia, which play a crucial role in motor control and reward processing, can also be affected, further complicating the behavioural manifestations of ADHD.
As research continues to unravel the neurological underpinnings of ADHD, it becomes evident that this disorder is not merely a behavioural issue but a complex interplay of biological, environmental, and genetic factors. Understanding these implications can guide the development of more effective interventions and treatments that address the neurological roots of ADHD, potentially improving outcomes for those affected.
Dopamine Dysregulation in ADHD
Dopamine dysregulation is a central theme in understanding ADHD, as it has profound effects on behaviour and cognitive function. Studies have shown that individuals with ADHD may have lower levels of dopamine in specific areas of the brain, particularly those involved in executive functions and reward processing. This deficiency can lead to difficulties in motivation and a heightened sensitivity to reward, often resulting in impulsive behaviours.
The concept of “reward deficiency” is particularly relevant in the context of ADHD. Individuals with ADHD may require more significant rewards or stimulation to achieve the same level of motivation or satisfaction as their peers without the disorder. This can manifest in behaviours such as seeking out novel experiences or engaging in risk-taking activities. Consequently, the drive for immediate gratification often overshadows the ability to plan for long-term goals, further exacerbating the symptoms associated with ADHD.
Moreover, the variability in dopamine receptor availability and functioning may contribute to the diversity of ADHD symptoms observed in different individuals. Some may experience predominant inattentive symptoms, while others may exhibit hyperactive-impulsive traits. These variations highlight the complexity of dopamine’s role in ADHD, indicating that therapeutic strategies targeting dopamine pathways must be tailored to individual profiles for effective management of the disorder.
Genetics and Dopamine Receptors in ADHD
Genetic factors play a significant role in the development of ADHD, with research indicating a hereditary component to the disorder. Variations in genes associated with dopamine receptors, particularly the D4 and D5 receptor genes, have been linked to an increased risk of developing ADHD. These receptors are crucial for mediating dopamine’s effects in the brain, influencing various cognitive and behavioural processes.
Polymorphisms in the dopamine transporter gene (DAT1) have also been implicated in ADHD. This gene regulates the reuptake of dopamine from the synaptic cleft, thereby influencing dopamine availability in the brain. Individuals with certain variants of this gene may experience altered dopamine signalling, contributing to the symptoms of ADHD. Understanding these genetic underpinnings is essential for identifying at-risk individuals and developing targeted treatment approaches.
The interplay between genetics and environmental factors further complicates the landscape of ADHD. While genetics may predispose individuals to the disorder, environmental influences such as prenatal exposure to toxins, early childhood trauma, and stress can exacerbate symptoms. This multifactorial approach highlights the need for comprehensive evaluations that consider both genetic and environmental contributions to ADHD, paving the way for personalised treatment strategies that address the unique needs of each individual.
Treatment Approaches for ADHD Targeting Dopamine
Given the strong link between dopamine dysregulation and ADHD, treatment approaches often focus on enhancing dopaminergic activity in the brain. Stimulant medications, such as methylphenidate and amphetamines, are commonly prescribed to individuals with ADHD. These medications work by increasing the availability of dopamine in the synaptic cleft, thereby improving attention and reducing impulsivity.
While stimulant medications are effective for many, they are not suitable for everyone and may come with side effects. As a result, non-stimulant options, such as atomoxetine, have been developed. Atomoxetine selectively inhibits the norepinephrine transporter, leading to increased norepinephrine and indirectly enhancing dopamine levels in the prefrontal cortex. This approach provides an alternative for individuals who may experience adverse effects from stimulants or have a history of substance use.
In addition to pharmacological interventions, behavioural therapies that focus on cognitive-behavioural strategies can also be beneficial. These therapies aim to develop coping mechanisms and organisational skills, helping individuals manage their symptoms more effectively. Combining medication with behavioural interventions can create a comprehensive treatment plan that addresses both the neurological and behavioural aspects of ADHD, improving overall functioning and quality of life.
The Link Between Dopamine and ADHD Symptoms
The link between dopamine and the various symptoms of ADHD is well-documented, with research indicating that dopaminergic dysfunction can manifest as inattention, hyperactivity, and impulsivity. Inattention may arise from insufficient dopamine signalling in the prefrontal cortex, which is responsible for executive functions such as planning, prioritising, and maintaining focus. As a result, individuals may struggle to sustain attention on tasks, leading to difficulties in academic and occupational settings.
Hyperactivity and impulsivity are also closely tied to dopamine levels. Increased dopaminergic activity in certain brain regions can lead to heightened arousal and restlessness, fuelling hyperactive behaviours. Impulsivity, characterised by hasty actions without forethought, may stem from an inability to regulate dopamine-driven reward-seeking behaviours effectively. As individuals with ADHD often experience a strong desire for immediate gratification, they may engage in impulsive actions to satisfy their needs, further complicating their ability to function in structured environments.
Understanding this connection between dopamine and ADHD symptoms is crucial for developing effective interventions. By targeting the underlying dopaminergic mechanisms, clinicians can better tailor treatments to address the specific symptoms experienced by individuals with ADHD. This nuanced understanding allows for a more comprehensive approach to managing ADHD, emphasising the importance of addressing both behavioural and neurological factors.
Neurotransmitter Imbalance in ADHD
Neurotransmitter imbalance is a hallmark of ADHD, with dopamine being one of the key players in this intricate network. While dopamine dysregulation is often emphasised, other neurotransmitters such as norepinephrine and serotonin also contribute to the overall picture of ADHD. An imbalance among these neurotransmitters can lead to a range of symptoms that affect behaviour, mood, and cognitive function.
Norepinephrine, for instance, plays a significant role in attention and arousal. Individuals with ADHD may exhibit lower levels of norepinephrine, which can further exacerbate difficulties in sustaining attention and regulating impulses. This interplay between dopamine and norepinephrine highlights the importance of considering multiple neurotransmitter systems when evaluating ADHD and its treatment options.
Additionally, serotonin, often associated with mood regulation, may influence emotional dysregulation commonly observed in individuals with ADHD. Fluctuations in serotonin levels can contribute to mood swings, anxiety, and irritability, which may co-occur with ADHD symptoms. By addressing the various neurotransmitter imbalances, clinicians can develop more effective treatment strategies that target the multifaceted nature of ADHD, ultimately improving patient outcomes.
Research Findings on Dopamine and ADHD
Research on the relationship between dopamine and ADHD has expanded significantly over the years, yielding valuable insights into the disorder’s neurobiological underpinnings. Neuroimaging studies have consistently shown altered dopamine receptor densities and availability in individuals with ADHD, particularly in brain regions associated with reward and executive function. These findings support the notion that ADHD is not merely a behavioural issue but a complex neurological condition influenced by neurochemical imbalances.
Longitudinal studies have also provided evidence for the role of dopamine in the development and persistence of ADHD symptoms over time. Children with ADHD who exhibit lower dopamine levels are more likely to experience persistent symptoms into adolescence and adulthood. This underscores the importance of early identification and intervention, as addressing dopamine dysregulation early on may mitigate the long-term impact of ADHD on an individual’s life.
Furthermore, ongoing research is exploring the potential for new treatment modalities that target the dopaminergic system more precisely. Advances in pharmacogenomics may soon allow clinicians to tailor medications based on an individual’s genetic profile, optimising treatment efficacy while minimising side effects. As research continues to unravel the complexities of dopamine and ADHD, it holds promise for developing innovative and effective strategies for managing this challenging disorder.
Conclusion and Future Implications
The connection between ADHD and dopamine is a fascinating area of study that continues to evolve as our understanding of neurobiology deepens. The interplay between neurotransmitter systems, genetic factors, and environmental influences underscores the complexity of ADHD and highlights the need for a multifaceted approach to treatment. As research progresses, it is crucial to remain open to new findings that may reshape our understanding of this disorder and its management.
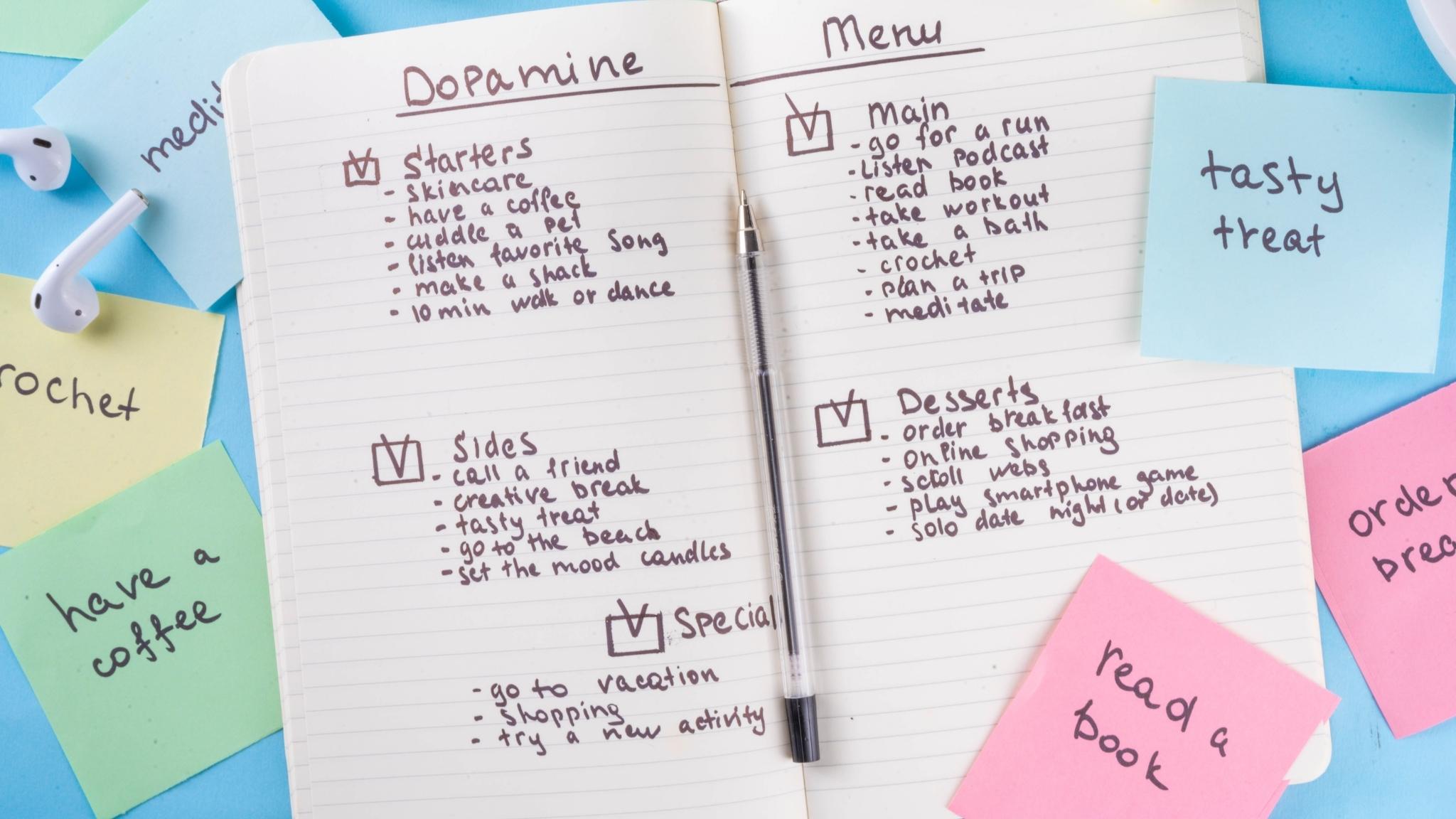
Future implications include the potential for personalised medicine approaches that consider individual differences in dopaminergic function and receptor profiles. By tailoring interventions based on these neurobiological factors, healthcare providers can enhance treatment outcomes and improve the quality of life for individuals with ADHD. Additionally, continued exploration of non-pharmacological interventions, such as behavioural therapies and lifestyle modifications, will be essential for providing comprehensive care.
As we move forward, fostering collaboration between researchers, clinicians, and patients will be key to advancing our understanding of ADHD and its connection to dopamine. By working together, we can develop more effective strategies for diagnosis, treatment, and support, ultimately empowering individuals with ADHD to thrive in their personal and professional lives. The journey to uncover the intricacies of ADHD and dopamine is ongoing, and the future holds promise for those impacted by this complex disorder.
